
Discover what’s next for AI in healthcare in 2026 - Get Access to the Full Report
2026 Global AI in Healthcare Report: A Playbook for HealthTech Leaders
Read on to unlock insights, trends, and strategies shaping the next phase of AI adoption in global healthcare.

On this page
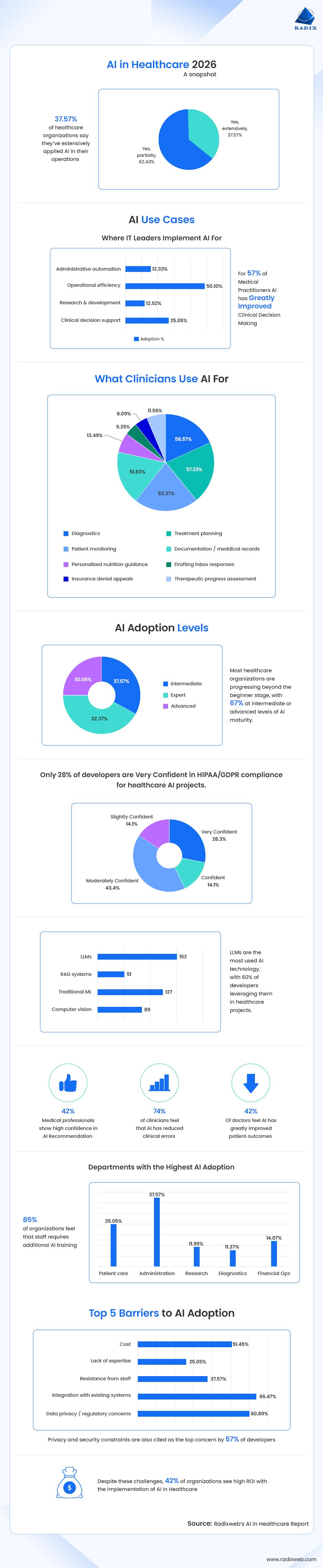
Executive Summary: Healthcare is entering its first true AI-native decade. What began as pilots in clinical decision support or admin automation is evolving into deeper, more reliable, workflow-integrated AI ecosystems. Radixweb’s 2026 Healthcare AI Report reveals a sector past experimentation and now focused on real ROI, efficiency, and measurable clinical impact.
| 750+ Participants | 4 Continents | 50,000+ Data Points |
|---|---|---|
| Participants including AI developers, healthcare practitioners & IT leaders | Continents including Asia, Europe, North America, and South America | Analyzable data points derived across all questions and response categories |
Key Findings
- 57% of clinicians say AI has greatly improved clinical decision-making.
- 58% use AI for diagnostics, the highest area of clinical adoption.
- More than 85% of clinicians believe they need additional training to use AI effectively.
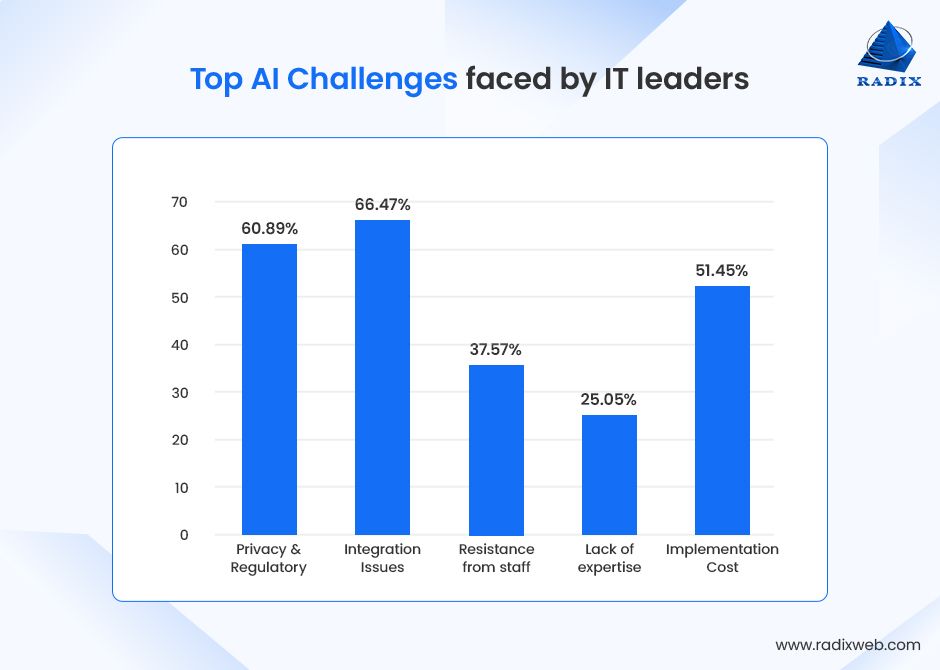
- 66% of healthcare IT leaders cite integration with existing systems as a top adoption barrier.
- 42% of organizations have achieved high ROI from AI initiatives.
- 37% of organizations already use AI extensively, and adoption continues rising.
- 43% of clinicians report AI has moderately reduced error rates, which is a strong early indicator of clinical safety benefits.
- 50% of healthcare operations use AI for efficiency-driven workflows such as scheduling, RCM, documentation, and automation.
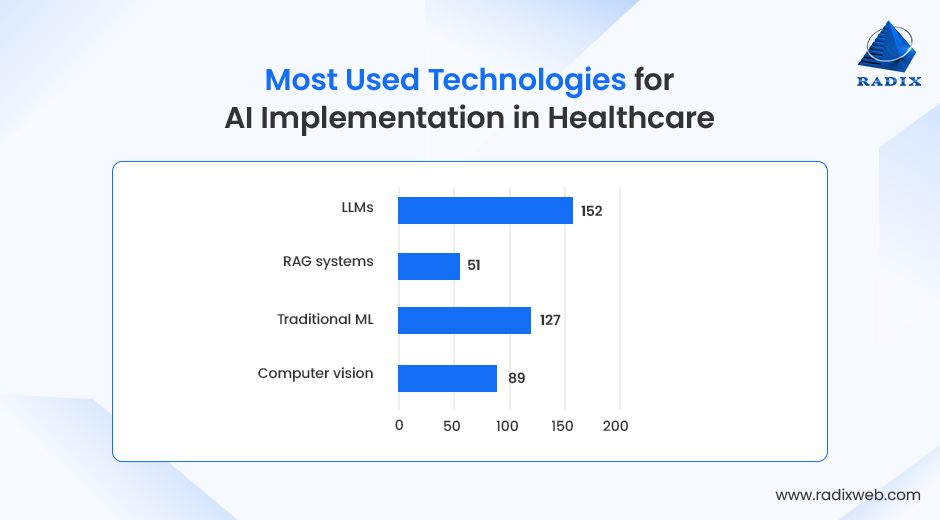
- LLMs are the most used AI technology, used by 60% of developers.
- RAG systems adoption is growing with 20% developers using it, while traditional ML are still being used by 50%.
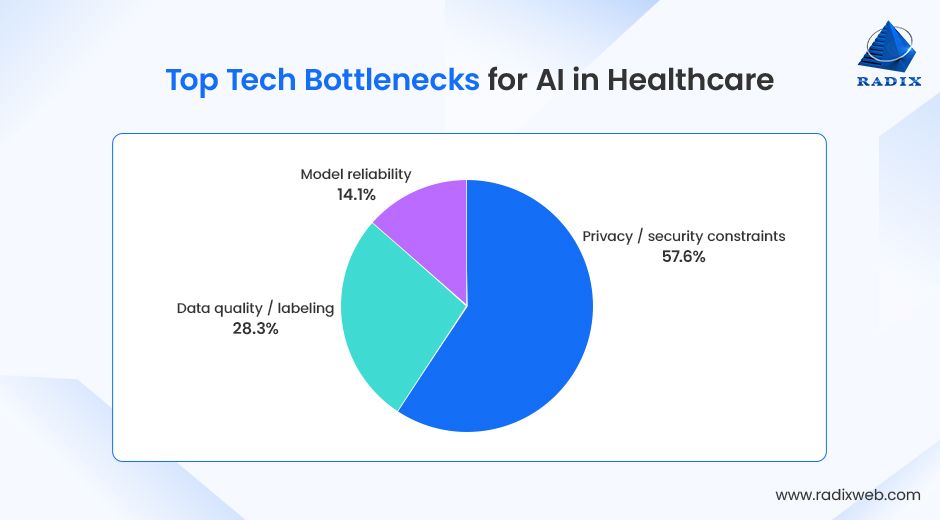
- Privacy/security constraints are the top concern among 57% of developers.
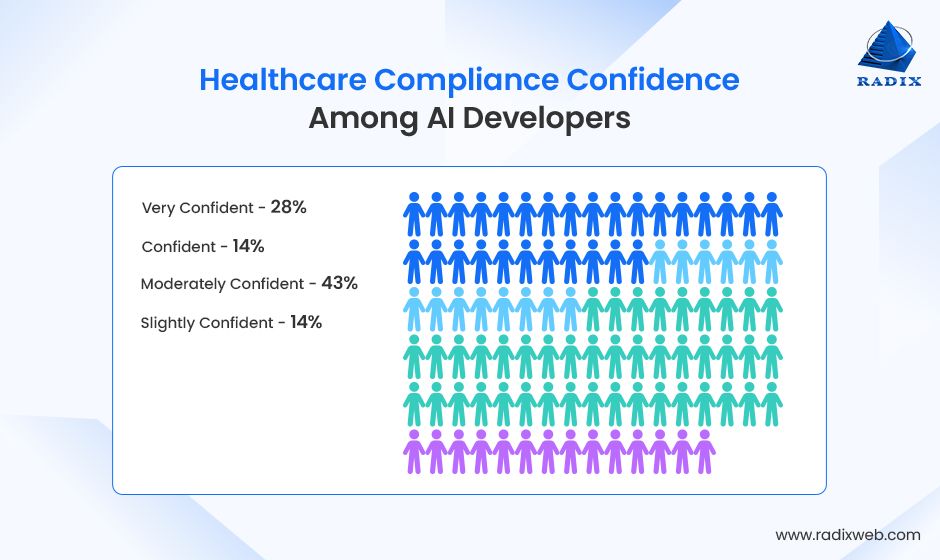
- 43% of developers report moderate confidence (3/5) in healthcare compliance.
The 2026 Outlook:
Healthcare moves from “AI-assisted” to AI-integrated, where automation, decision support, multimodal patient modeling, and administrative AI become core infrastructure.
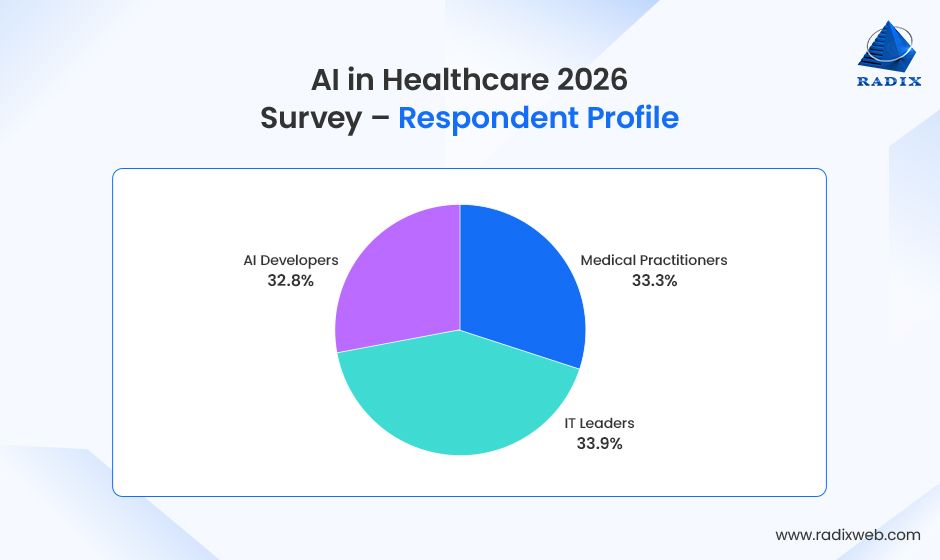
Methodology & Respondent Profile
This report explores how AI is transforming healthcare, from clinical decisions to operational efficiency. Radixweb conducted this study at a pivotal moment: 2026 marks a shift as AI moves from pilots to fully integrated, clinical-grade systems. With insights from both clinicians and IT leaders, the report highlights adoption trends, barriers, and opportunities, providing a clear picture of where healthcare AI is today and where it’s headed.
Sample Overview
This report draws insights from respondents across the healthcare ecosystem, comprising:
- 257 medical practitioners: physicians, specialists, clinicians, and care coordinators
- 262 senior healthcare IT leaders: CIOs, CTOs, digital transformation leaders, IT directors, system architects, and operations executives
- 253 AI developers: ML engineers, data scientists, algorithm specialists, prompt engineers, and software architects
Respondents shared detailed inputs across the following dimensions:
- Clinical use of AI: decision support, diagnostics, monitoring, documentation
- Operational and administrative applications: workflow automation, revenue cycle, resource optimization
- Adoption maturity: implementation depth, AI readiness, departmental adoption
- Impact measurement: efficiency gains, error reduction, workflow changes, ROI
- Barriers and risks: regulatory concerns, integration gaps, staffing challenges
- Confidence and trust: clinician comfort, reliability of AI recommendations
- Future outlook: priorities, investment areas, organizational expectations
Data Collection Approach
Data was gathered through a structured questionnaire including:
- Single-choice questions
- Multi-select questions
- Likert-scale confidence and impact ratings
- Open-ended experience-based responses
All findings reflect direct responses from the 519 participants, ensuring balanced representation between clinical and IT domains.
Chapter 1: The State of AI in Healthcare 2026
Healthcare in 2026 stands at a turning point: after years of experimentation, AI has moved firmly into the fabric of clinical and operational workflows. What began as a series of pilots and isolated use cases has matured into broad adoption across hospitals, clinics, and health systems. The tone of the industry has now shifted from “Will AI work?” to “How do we scale what’s already working?”
On the ground, this shift is unmistakable. Across organizations, leaders are no longer debating whether AI belongs in healthcare. Earlier studies showed that 26% of healthcare organizations are yet to consider AI solutions. But every respondent in our study reported active AI implementation, with most using it to enhance daily operations and support decision making.
AI is now embedded in the everyday tasks that determine whether systems run smoothly:
- Diagnostics (58.57%)
- Treatment planning (57.23%)
- Patient monitoring (53.37%)
- Documentation/medical records (51.83%)
- Personalized nutrition guidance (13.49%)
- Drafting inbox responses (9.25%)
- Insurance denial appeals (8.09%)
The percentages in parentheses represent the proportion of respondents who selected that option. Respondents could choose more than one option, so the percentages do not sum up to 100%.
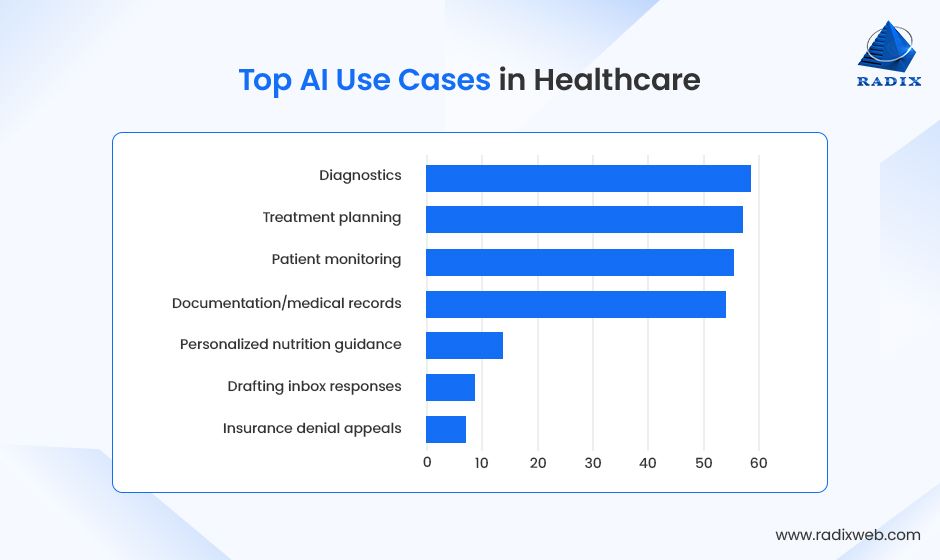
This is the quiet but significant transformation of 2026 – The normalization of AI in frontline work.
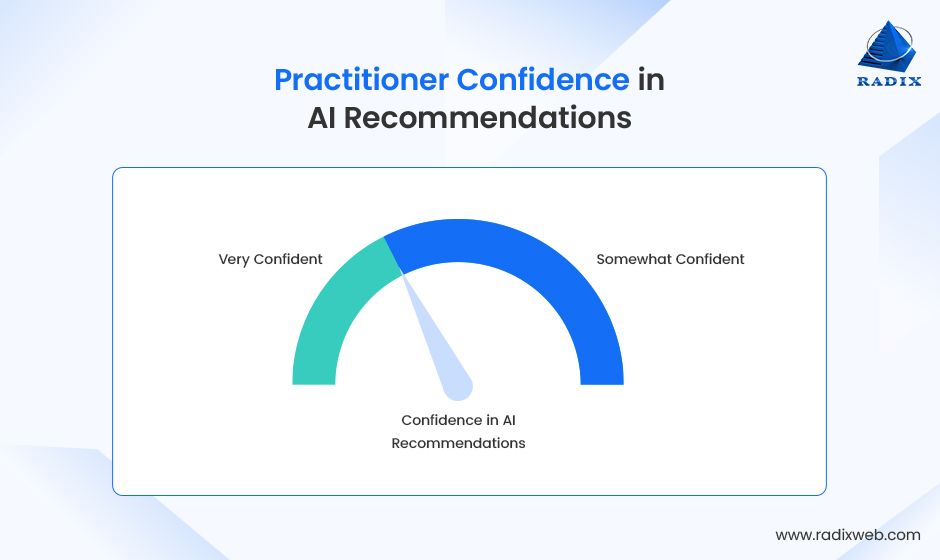
What's more important is that now clinicians increasingly view AI not as a novelty but as a practical instrument that improves care. Many respondents (42.58%) show strong confidence in AI recommendations, which have resulted in greater accuracy in treatment planning, more reliable monitoring of patients, and smoother documentation.
The majority say that AI meaningfully improves their decision-making and daily workflow. That’s an important signal that clinical AI is moving beyond early-stage hyper into measurable impact.
Still beneath the momentum lie structural tensions that the industry must confront. Most clinicians acknowledge that AI demands new forms of capability, with more than 85% of them saying that the staff does need some sort of AI training.
IT leaders, on the other hand, continue to grapple with integration challenges (66%), regulatory constraints (60%), staff resistance (37%), and high costs of AI implementation (51%).
Overall, the maturity of AI system is rising quickly. But the maturity of organizations to deploy them safely and at scale has not kept pace. This asymmetry will shape the next phase of AI’s evolution.
Future Outlook
What makes 2026 pivotal is not simply what AI is doing today. Instead, it is what the next five years are poised to unlock. Advances in multimodal models, clinical-grade AI systems, digital diagnostics, ambient clinical intelligence, and automated administrative infrastructures are transforming the expectations of what is possible. By 2030, three shifts are likely to define healthcare AI’s trajectory.
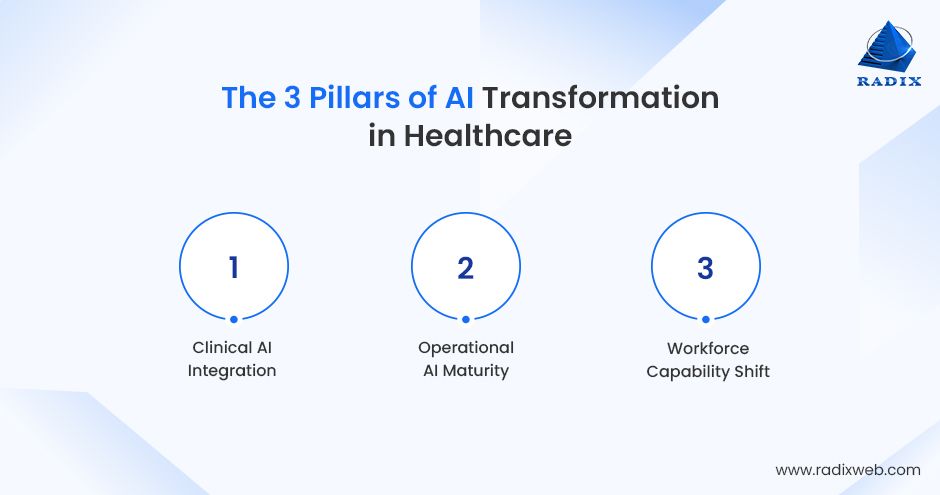
First, AI will become a core layer of clinical decision-making, not just an assistive tool.
With models capable of interpreting imaging, labs, genomics, and longitudinal patient histories, care teams will increasingly rely on AI to surface risks earlier, personalize treatments, and reduce diagnostic variability.
Second, operational AI will reach full maturity, reshaping how hospitals run.
End-to-end automation, spanning claims management, care coordination, scheduling, and documentation, will free up thousands of hours of administrative work and help systems regain financial stability.
Third, the workforce will undergo a capability shift.
It will happen as clinicians and administrators develop AI literacy and organizations adopt governance frameworks that ensure safe, equitable deployment. The institutions that learn to adapt quickly will capture the majority of AI’s value.
Taken together, the state of AI in 2026 is defined by momentum, not maturity.
It is a sector in motion. It is advancing rapidly, solving real problems, and reshaping the contours of modern healthcare. What emerges by 2030 will depend not only on model innovation but on whether health systems can develop the infrastructure, talent, and trust needed to scale AI responsibly and effectively.
On the imperative of responsible AI adoption, Mr. Divyesh Patel, CEO of Radixweb, notes...

Chapter 2: Key AI Applications in Healthcare
AI is increasingly embedded across a wide range of healthcare activities, enhancing clinical decision-making, streamlining workflows, and supporting administrative tasks. Our study reveals which applications are seeing the most adoption and where value is being realized.
Treatment Planning
In treatment planning, 57% of clinicians use AI to develop personalized care strategies.
A strong example comes from First Ascent Biomedical, where platforms combining tumor cell testing, genomic data, and AI analysis can return ranked treatment options within days. The approach showed an 83% patient benefit rate with their Functional Precision Medicine (FPM) platform, which brings together tumor cell testing, genomic profiling, and AI to identify which therapies are most likely to work for each individual patient.

By integrating patient histories, lab results, and AI predictive analytics, clinicians can choose the most effective treatment plans, reducing trial-and-error approaches, and improving patient outcomes.
Diagnostics
AI is helping clinicians identify conditions more accurately and quickly. Nearly 59% of medical practitioners report using AI for diagnostics. It is being leveraged for imaging interpretation, lab data analysis, and predictive modeling to detect abnormalities that may otherwise go unnoticed. This application is becoming a foundational tool for early detection and preventive care.
Patient Engagement
AI imaging tools are also helping clinicians visually explain conditions and symptoms to patients, improving understanding and trust. Dr. David Ghozland, who specializes in cosmetic gynecology, for example, explains that he uses AI imaging tools to study tissue and blood vessel patterns before performing laser treatments or surgery.

Documentation/Medical Records
Managing clinical documentation is time-consuming, but AI is helping to streamline this process. 53% of clinicians use AI to automate record-keeping, generate notes, and maintain accurate patient records. This not only reduces administrative burden but also improves data quality and allows clinicians to focus more on direct patient care.
Patient Monitoring
AI supports continuous monitoring of patient health, alerting clinicians to early warning signs and deviations in real-time. 53% of practitioners report using AI for patient monitoring, from chronic disease management to post-operative follow-up. This has enabled proactive interventions that improve safety and reduce complications.
As Dr. Eleni Nicolaou, Art Therapist & Creative Wellness Expert, explains, AI can identify subtle stress indicators long before they become outwardly visible.

Personalized Guidance
AI is increasingly applied in preventive and precision medicine, including personalized nutrition advice. Around 13% of clinicians report using AI to tailor dietary recommendations for chronic conditions and metabolic health, highlighting emerging use cases beyond traditional diagnostics and treatment.
Drafting Inbox Responses
Some clinicians are using AI to assist with routine communication tasks, such as drafting responses to patient messages. While still limited (9% adoption), this application demonstrates AI’s potential to reduce administrative friction and improve responsiveness in patient interactions.
Insurance Denial Appeals
A smaller but meaningful subset of clinicians (8%) use AI to support insurance denial appeals, automating document review, identifying policy inconsistencies, and generating evidence-based responses. This extends AI’s value beyond clinical care into the administrative and financial tasks that often drain staff time and delay patient access to services.
Elise Dreiling, CPO and Director of Clinical Operations at Open Bionics, notes that many insurance policies still rely on outdated evidence, adding that she often must “respond with current, peer-reviewed studies specific to multi-grip myoelectrics.”
Her team has seen about a 50% approval rate on appealed denials, underscoring how AI-assisted evidence gathering and document preparation can help clinicians navigate complex, sometimes restrictive, coverage policies.

The breadth of these applications shows that AI is becoming an integrated component of modern healthcare. The adoption patterns reflect both the immediate impact of AI and the potential for future expansion.
Chapter 3: Divergence & Alignment: Where IT Leaders’ and Clinicians’ Priorities Clash and Converge
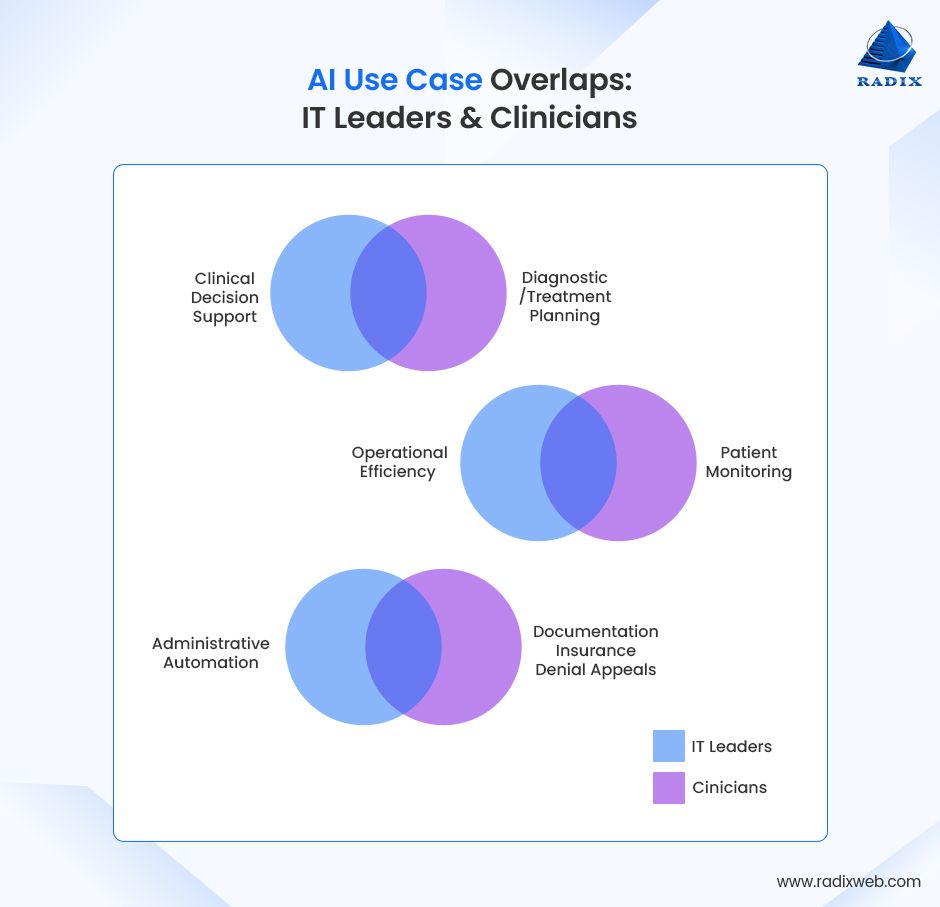
The study reveals a clean and compelling reality: AI is reshaping healthcare from two very different vantage points.
As our COO, Mr. Dharmesh Acharya sums it up,

Despite this contrast, the data also shows areas of consensus. The alignment highlights where healthcare organizations can move quickly. The divergence points to structural gaps that must be addressed for AI to scale responsibly.
Where IT Leaders and Clinicians Align on the Use of AI in Healthcare
Across both groups, the following three areas of strong agreement emerge.
1. Both groups recognize AI as a net positive for performance.
While IT leaders point to system-level gains in efficiency and ROI, clinicians report improvements in decision-making and workflow speed. The shared sentiment, however, is unmistakable: AI is already delivering measurable value within hospitals and care settings.
2. Both see AI as a capability that requires significant workforce readiness.
Clinicians overwhelmingly express the need for further training, and IT leaders raise concerns about organizational expertise and staff resistance. Both sides understand that AI maturity is not just a technology challenge, it is a skills, culture, and adoption challenge.

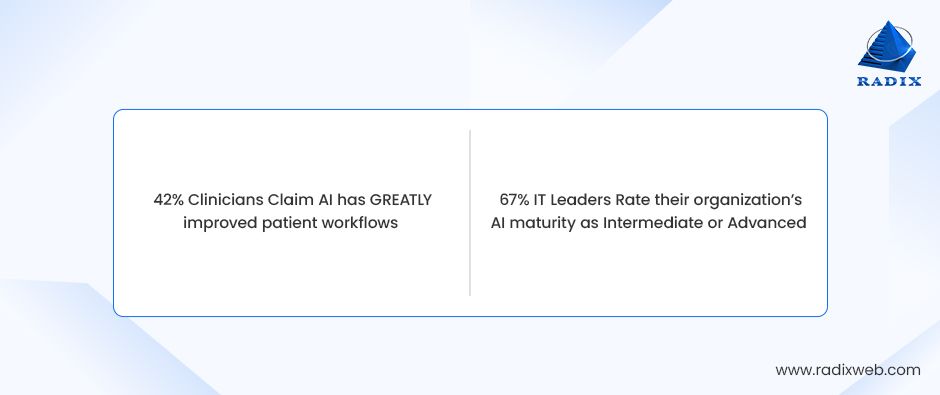
3. Both acknowledge that AI is moving from experimental to operational.
IT teams report intermediate to advanced levels of AI maturity, and clinicians claim that AI has greatly improved patient workflows. The consensus is that AI is no longer a pilot initiative but a core component of modern care delivery.
Together, these alignment points provide a strong foundation for accelerated transformation.
Where They Diverge: The Two Sides of the Same Coin
Beneath the shared optimism, however, the study uncovers fundamental differences in priorities and lived experience.
Here’s how that difference in vision becomes clear:
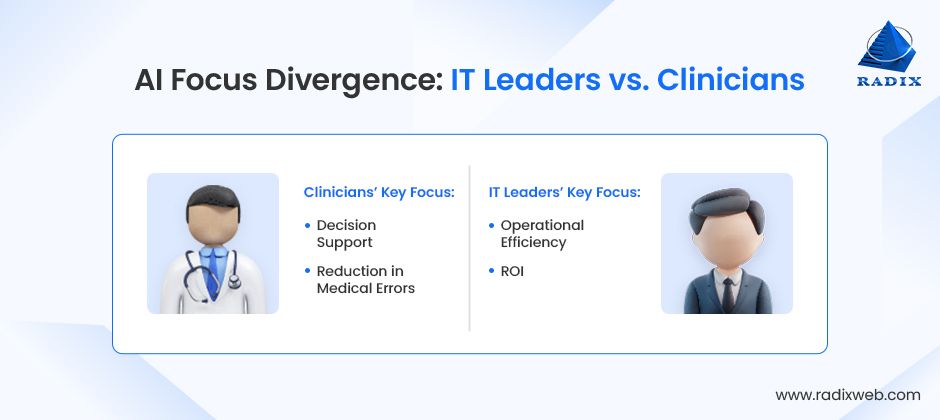
1. IT leaders emphasize scaling while clinicians emphasize trust
Operational efficiency is the top AI priority for IT leaders. But clinicians place greater weight on diagnostic accuracy and care quality. While IT leaders see AI as an enterprise-wide efficiency engine, clinicians see it as a decision-support companion whose recommendations must be explainable and reliable.
2. IT leaders are confident in ROI; clinicians are ambivalent about clinical risk
Nearly all IT leaders report medium to high ROI from AI investments. Clinicians, on the other hand, are not as unanimous on whether AI has reduced medical errors. This underscores a key tension between perceived financial return and perceived clinical safety.
These divergences do not indicate disagreement but instead reflect two different (but equally necessary!) perspectives within healthcare. Each group sees a different dimension of the same transformation.
Closing the Gap: A Shared Path Forward
As AI shifts from innovation to infrastructure, tension naturally emerges between system-wide goals and frontline realities. The opportunity lies in using this divergence as a navigational tool.
Bridging the gap will require governance models that integrate clinical oversight, technology roadmaps anchored in patient outcomes, and enterprise investments that elevate both digital capability and clinical trust. When these two perspectives converge, healthcare organizations unlock the full power of AI.
Chapter 4: The Big Barriers: What’s Preventing Healthcare AI From Scaling
Even as AI becomes more embedded in healthcare operations, technology leaders report a consistent set of barriers that limits its ability to scale beyond departmental pilots. Here are the biggest barriers at the moment:
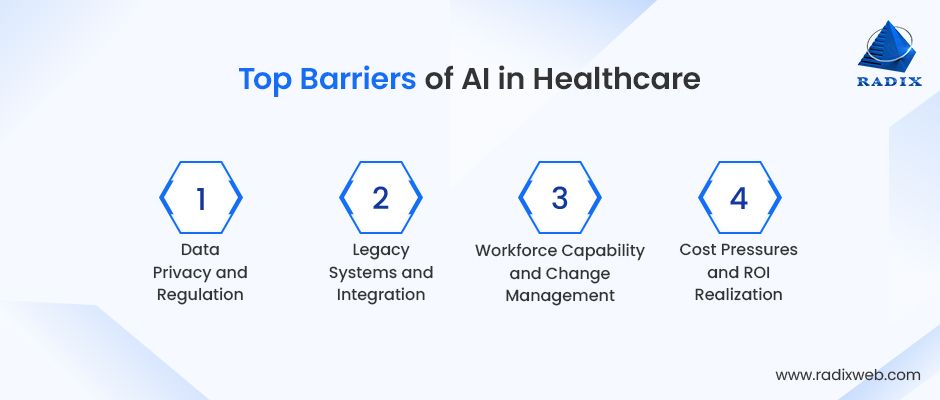
Data Privacy and Regulation
60% of IT leaders cite data privacy and regulatory concerns as one of their biggest barriers, making it the most widely reported challenge.
This reflects an environment where the speed of AI innovation is outpacing the clarity of regulatory guidance. With new expectations around clinical-grade AI systems, auditability, and explainability, organizations are required to strengthen their governance frameworks before expanding use cases.
Legacy Systems and Integration
An even large share (66%) say integration with existing systems is a major obstacle.
Healthcare technology environments are highly fragmented, with decades-old EHR platforms, siloed operational tools, and custom-built internal systems. AI solutions, even when clinically validated, struggle to integrate smoothly into this diverse ecosystem.
As long as AI systems operate adjacent to (rather than inside) core clinical and administrative workflows, their impact will remain limited. Scaling AI is as much an infrastructure modernization effort as it is an innovation initiative.
Workforce Capability and Change Management
While IT leaders point to resistance from staff (37%) and lack of expertise (25%) as barriers, clinicians reinforce this challenge from the frontline. A striking 85% of clinicians say staff require additional AI training, even though nearly all agree that AI has improved their decision-making and workflow efficiency.
Dr Maria Knobel, from MedicalCert, also warns about incorrect inputs from medical staff which result in false signals during her remote triage and preventive assessment sessions. She says,

This signals a workforce that sees value in AI but is not yet fully prepared to use it with confidence. Adoption is happening, but capability-building and change management are lagging behind the technology curve
Cost Pressures and ROI Realization
Despite strong returns (42% of IT leaders report high ROI and 38% moderate ROI) 51% still identify cost as a barrier to broader adoption.
Dr. Rron Bejtullahu from SonderCare perfectly sums up this contraction when he explains their use of AI tools for eye exams. He says,

This makes it clear that the issue is not whether AI delivers value. It definitely does.
The challenge, however, is that this value is not always immediate, evenly distributed, or easily measurable across departments. And AI requires sustained investment in data infrastructure, integration, governance, and training before returns become visible at scale.
For many organizations, this creates a timing mismatch between investment cycles and impact cycles.
The barriers identified by IT leaders reveal a system that is eager for innovation but constrained by foundational gaps. The path forward requires not just new AI tools, but new regulatory readiness, new infrastructure, new workforce capabilities, and new financial models. Organizations that treat AI scaling as an enterprise-wide modernization effort not merely a technology rollout, will emerge the furthest ahead.
Chapter 5: Inside the Build: AI Developers’ Perspective on Healthcare AI in 2026
If clinicians define whether AI is useful and IT leaders decide whether it is scalable, AI developers determine whether healthcare AI is even possible.
Below we’ve captured the voices of engineers, data scientists, and AI architects who are actively building healthcare AI systems in production environments. These are the teams wrestling with real patient data, real regulatory constraints, and real consequences when systems fail. Their responses reveal a critical truth about healthcare AI in 2026:
The technology is advancing faster than the foundations required to deploy it safely and at scale.
1. The Technology Stack Powering Healthcare AI Today
Healthcare AI systems are built using multiple AI technologies working together. Developers commonly combine LLMs, traditional machine learning, computer vision, and retrieval systems to meet clinical, operational, and compliance needs. The focus is on reliability and real-world usability, not experimentation.
2. The Real Bottleneck Isn’t Innovation. It’s Constraint.
The biggest challenge in healthcare AI is operating within privacy, security, and regulatory limits. Data quality issues and reliability concerns further slow progress. In practice, compliance and infrastructure shape AI systems more than model capability does.
3. Compliance Confidence: Strong, But Not Absolute
Developers express moderate confidence in building HIPAA- and GDPR-compliant AI systems. Most acknowledge that compliance is complex, evolving, and difficult to scale consistently. It is viewed as an ongoing engineering responsibility, not a one-time requirement.
4. Where Developers See the Greatest Risk
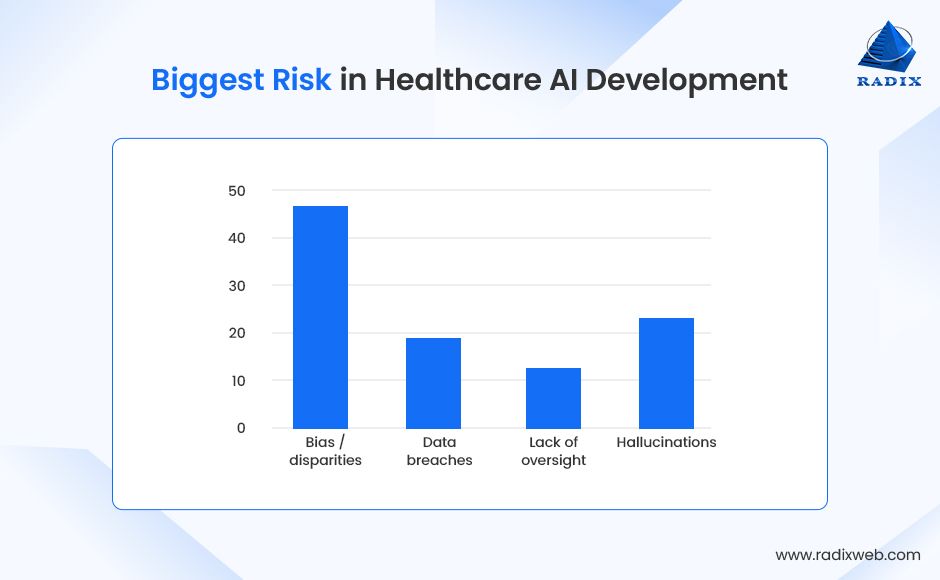
Developers identify bias and unequal outcomes as the highest risk in healthcare AI. Hallucinations, data breaches, and lack of oversight also raise concern, particularly where AI informs clinical decisions. Managing trust and accountability is as critical as model performance.
What This Means for Healthcare AI Leaders
Developers’ insights show that healthcare AI in 2026 is ready to deliver real impact. The technology works, the use cases are proven, and early results show meaningful improvements in care and operations.
Scaling AI successfully now is about doing the right things consistently:
- Build systems that are compliant and secure from the start.
- Use high-quality, connected data so AI decisions are reliable.
- Design AI to reduce bias and improve outcomes for all patients.
- Set up governance across teams so clinical, operational, and tech goals align.
Organizations focusing on these areas will not just implement AI—they will get measurable results, improve workflows, and enhance patient care.
Healthcare AI is moving from experimentation to everyday practice. Those who invest in strong foundations today are shaping the future of care for 2030 and beyond.
Radixweb Health AI Matrix 2026: A Practical Roadmap for Healthcare Leaders
As the findings of this study show, healthcare organizations are moving toward AI adoption with very different levels of readiness, clarity, and measurable progress. These variations make it challenging for leaders to understand their true position in the broader transformation landscape. And even harder to decide what to prioritize next.
To offer a clear, structured way forward, we developed the Health AI Matrix 2026. This matrix serves as a practical decision-support tool that helps organizations locate themselves on the AI maturity map, assess the value they are currently capturing, and chart a realistic path toward higher-impact, system-wide enablement.
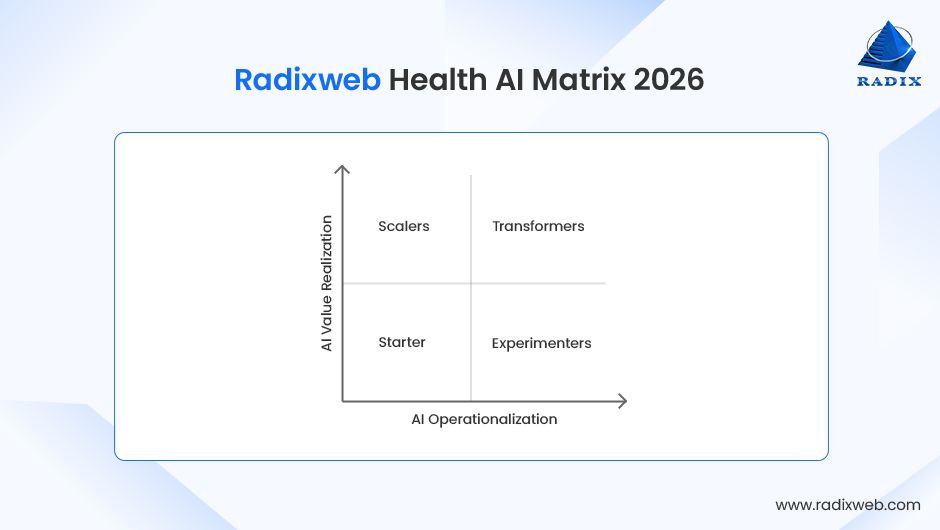
What the Matrix Measures
The matrix evaluates healthcare organizations across two dimensions essential for successful AI enablement:
1. AI Operationalization (X-axis)
How effectively AI is embedded into real workflows and not just in pilots, but across clinical, operational, and patient-facing journeys.
Low → High reflects:
- Data readiness
- Workflow integration
- Automation enablement
- Governance & compliance maturity
- Interoperability quality
2. AI Value Realization (Y-axis)
The extent to which the organization is achieving measurable outcomes from AI.
Low → High reflects:
- Efficiency gains
- Cost savings
- Reduced clinician burden
- Improved patient outcomes
- Scalable ROI across departments
The Four Quadrants: Where Healthcare Organizations Stand Today
Healthcare AI maturity today can be mapped across four actionable quadrants.
| Scalers (High Operationalization, Emerging Value) | Transformative Performers (High Operationalization, High Value) |
|---|---|
| These are the teams that have built the right foundation and are now expanding with: • AI governance in place • Multiple departments using AI • Early ROI signals visible If you are here: Double down on cross-functional adoption, clinician alignment, and system-wide automation. | A small but growing segment of organizations where AI is a core operational capability. • AI as a clinical co-pilot • Predictive & prescriptive systems • Measurable enterprise-wide ROI If you are here: Focus on continuous improvement, advanced models, and enterprise orchestration. |
| Starters (Low Operationalization, Low Value) | Experimenters (Low Operationalization, High Activity) |
|---|---|
| Most common among small practices and early-stage hospitals. • Minimal data unification • Few automation-ready workflows • AI limited to exploration If you are here: Focus on foundational upgrades like AI integration in EHR/EMR, interoperable data, and small repeatable automations. | Organizations piloting AI tools in isolation often find themselves here. • Innovation teams active • Fragmented experiments • No enterprise ROI If you are here: Prioritize workflow integration over adding more pilots. In short, focus on consolidating, standardizing, and establishing governance standards. |
How To Use the Radixweb Health AI Matrix 2026
To make the matrix even more actionable, leaders can use a simple scoring framework to self-assess their organization’s maturity.
Rate your organization on the statements below using a 1–5 scale:
- 1 = Not true at all
- 5 = Fully true
AI Operationalization Score (X-Axis)
| Statement | Enter number (max 5 digits) |
|---|---|
| Our data is interoperable, unified, and reliable enough for AI use. | |
| AI systems are integrated with existing EHR/clinical workflows. | |
| We have clear AI governance, compliance, and audit standards. | |
| Departmental teams consistently use AI tools (clinical or operational). | |
| We have automation-ready workflows across multiple functions. |
Total Operationalization Score (Max 25): 0
AI Value Realization Score (Y-Axis)
| Statement | Enter number (max 5 digits) |
|---|---|
| AI has demonstrably reduced clinician or staff workload. | |
| AI-driven workflows have improved efficiency or throughput. | |
| We can quantify financial ROI or cost savings from AI. | |
| AI applications have improved patient outcomes or safety. | |
| AI value is visible across multiple departments, not just isolated teams. |
Total Value Score (Max 25): 0
How to Interpret Your Scores
Use the guide below to determine your quadrant:
- 0–12 on both axes → Starters
You are early in the AI journey. Focus on foundational upgrades and small-scale operational wins.
- Operationalization 13–25, Value 0–12 → Scalers
Your groundwork is strong. Now prioritize cross-functional adoption and measurable ROI.
- Operationalization 0–12, Value 13–25 → Experimenters
You’re piloting actively but not integrating. Consolidate, standardize, and govern before expanding.
- 13–25 on both axes → Transformative Performers
You’re achieving system-wide AI value. Focus on advanced models, orchestration, and continuous optimization.
What Comes Next: A 2030 Outlook for AI in Healthcare
By 2030, the AI in healthcare market will be worth 208.2 billion. AI will be poised to become a core infrastructure of healthcare systems rather than an auxiliary tool. The next five years will see wider deployment of clinical-grade AI models capable of interpreting multimodal data allowing for truly personalized and predictive care. Yet adoption alone will not define success.
The future of AI in healthcare depends on building trust, transparency, and explainability into every application. Clinicians and patients alike will expect systems that are reliable, interpretable, and ethically aligned with care objectives. At Radixweb, we are ready to support healthcare providers in navigating this shift, helping implement AI solutions that are secure, scalable, and aligned with both operational and clinical priorities. With 25+ years of experience and multiple healthcare and AI projects delivered, we have what it takes to deliver AI solutions that will not just keep you in-sync with the trends, but ahead of the industry curve.
With a 30-minute strategy session to see how you can use AI in 2026
