Read More

Discover what’s next for AI in healthcare in 2026 - Get Access to the Full Report
ON THIS PAGE
Summary: In the age of digital boom, AI-led capabilities aren’t just trendy. They are crucial for next-gen efficiency. But when it comes to having AI-powered healthcare and medical records, many business leaders hesitate. Today we’ll try to simplify why traditional EHRs and EMRs do not work anymore and why AI integrations are necessary. Read on.
In the age of modern healthcare, digital records like EHRs (Electronic Health Record) and EMRs (Electronic Medical Record) have been around for a while. In fact, the US government had incentivized the use of EHR systems in its HITECH and ARRA Acts of 2009.
However, the real picture says that adoption of these electronic record systems backfired for the healthcare industry. Healthcare professionals, already bogged with manual systems, received another round of frustration in the name of improved efficiencies.
This blog aims to dissect why traditional EHRs and EMRs didn’t make sense backed by realistic stats. I’ll also guide you with a modern take on improving operational efficiency in health tech. By the end of the piece, you’ll have a clear picture of why implementing AI in healthcare is necessary now and what you can do to make the process frictionless. Let’s drive straight in.
Why Did the Traditional Healthcare Record Systems Fail – Because They Overpromised and Underdelivered
The EHR integration was initially started with three distinct directions:
- Enhancing patient care
- Improving operational efficiencies
- Reduce healthcare and its operational costs
But in the bid for building safe digital healthcare systems, businesses ended up making sloppy executions. Healthcare practitioners, clinicians and support staff soon experienced the woes and burdens of:
- Fragmented workflows disrupted by ill-designed interfaces
- Difficulty of navigating complex healthcare systems
- Data overload, alert paralysis leading to missed diagnosis and care
- Widespread data vulnerabilities threatening patient privacy and loss of credibility in market
Furthermore, EHRs had highly complicated processes of recording and extraction of healthcare data. They required extensive manual data entry that ate into patient interaction tasks, changing the course of most healthcare job profiles into data entry clerks, leading to dissatisfaction and burnout.
Clearly, digital records weren’t doing their jobs right! And that’s where artificial intelligence stepped in.
AI in Digital Records – An Illusion or A Fresh Scope?
While adoption of digital record in healthcare failed miserably, they led to building the vast depository of data, which now is being used for healthcare AI solutions. Years of rich data capture by human workforces are helping AI models transform healthcare by unearthing patient usage patterns, foreseeing outcomes and enhancing critical decisioning.
Leveraging the power of structured data, healthcare businesses are now inching towards enhanced diagnostics, proactive, preventive and more personalized care, upskilling healthcare professionals and higher patient outcomes.
Key Benefits by integrating AI with EHRs and EMRs
Here are some noteworthy benefits of AI-enhanced EHR/EMR workflows:
Clinical Decision Support: Integrating AI with legacy EHRs help healthcare professionals foresee health risks in patients, forecast admission/readmission ratios and even predict contrary drug reactions on the basis of disease detection and early diagnosis of medical conditions.
Administrative Efficiency: Healthcare experts reportedly spend over 9 hours a week on EHR documentation. AI-led bots and assistants streamline data inventories with real-time inputs. AI integrations help convert manual records into digital data, streamlines billing, insurance claims, fraud detection etc.
Enhanced Interoperability and Patient Experience: AI-led systems promote interoperability by fostering frictionless data sharing with MLOps. From connection disparate EHR systems, unlocking easy management and exchange of patient data leading to more accuracy in documentation and thus, positive patient experiences.
AI app development has transformed several industries. However, its potential for the healthcare industry needs some digging. Let’s get on!
AI Integration in EHRs/EMRs Is No Longer Optional – Why?
Dr. Eric Topol, the founder of Scripps Translational Institute made a very interesting statement on AI-led EHRs. He stated that, “AI is only as good as the data it learns from—and EHRs are a goldmine of untapped insights.”
What we must understand here is that the scope of AI in healthcare has moved beyond digitization of records. Your medical record systems can deliver poignant results only when you decode the intelligence behind your systems, driving true digital transformation for healthcare. However, is you continue to operate in the ‘rich-in-data, poor-in-insights’ scope, you’ll be leaving out a lot of prospects.
Our COO, Dharmesh Acharya points out, “At Radixweb, we strive in delivering the most crucial value of AI – unlocking the ability to turn data into decisions. For healthcare, the way I see it, growth lies in transforming to predictive from reactive. By plugging AI in EHR, we aim to close the legacy – automation gap; enabling healthcare providers to deliver smart, seamless and personalized care.”
As per a report by Grand View Research, AI in the healthcare sector for US in 2024 was calculated in $13.26 billion. The latest projection expects it to grow at a CAGR of 36.76% by 2033, rapidly enhancing clinical outcomes, reshaping healthcare operations and rapidly transforming patient engagement rates. The problem, however, lies with legacy systems that do not fail in terms of agility but also in analytical strength required to power AI capabilities.
For 2025 and beyond, if your healthcare business wants to stay relevant, you can’t treat AI integrations like a mere upgrade or an industry trend – you have to pursue it like a strategic priority.
But knowing about trends and executing their implementation are two different ballgames. Get into the details with me!
How Does the AI-EHR/EMR Integration Landscape Look like?
In the context of EHR and EMR integrations, interoperability is the key to unlock possibilities. And the following integration approaches allow you to achieve that:
HL7 Integration: The most widely adopted integration standards in healthcare, Health Level Seven uses HL7 v2.x messaging for clinical data exchange. It helps build interoperability between EHRs, LIS, RIS etc. but has limited support for web APIs.
FHIR Integration: An amplified version of HL7, Fast Healthcare Interoperability Resources is a modern standard to streamline real-time data exchange with RESTful APIs and JSON/XML formats. It leverages resource-based architecture, OAuth 2.0, SMART on FHIR encryptions, supports cloud platforms, mobile integrations and advanced web technologies. Although it’s easier to implement than HL7 v2.x, data mapping from legacy HL7 formats become challenging.
API Integration: This facilitates connection between EHRs and third-party apps with custom and vendor-provided APIs. They use SOAP APIs and RESTful for frictionless data exchange between analytics, billing systems, telemedicine solutions. They are mostly preferred for specialized apps and custom workflows for real-time clinical decision support.
Mediated Integration: It centralizes integration logic with middleware and integration engines like Mirth Connect, Rhapsody. It also simplifies multi-system integration, handles routing and orchestration of messages, converts data formats and enhances error handling.
Cloud-Based Integration: It uses GCP, Azure, AWS cloud platforms to connects EHRs and EMRs with analytics, AI tools and other healthcare solutions. The best part is that it supports quick scalability, collaboration and data access across diverse locations. Cloud integrations are cost-effective, promote compliance adherence, and unlocks ML and analytics on data accumulated.
Native AI Models: These offer built-in integrators for EHRs offered by enterprise vendors that facilitate automated coding, risk predictors etc.
Custom AI Models: They offer capabilities built around your workflows and core patient needs to solve specific challenges which off-the-shelf solutions cannot solve.
Advanced AI Models: These are preferred by businesses that invest heavily in creating market differentiation. They involve Gen AI or building specialized models to deliver tailored capabilities for healthcare businesses.
Now that you’ve known about the various integration approaches, let’s give you a step‑by‑step AI in EHR/EMR integration guide on enabling this game-changing integration correctly.
Now you must be wondering how to integrate AI into existing EHR/EMR systems while maintaining business continuity. I have given a practical list down below.
Step-by-Step Process for Integrating AI Capabilities in EHRs and EMRs
AI in EMR and HER is supposed to make your systems more efficient for handling diverse market shifts and patient needs. However, you must remember that they have the capability to impact workflows, compliance adherence and patient experiences for better or worse.
To make the process risk-free and align seamlessly with existing workforce, you must follow these best practices for AI and EHR/EMR system Integration.
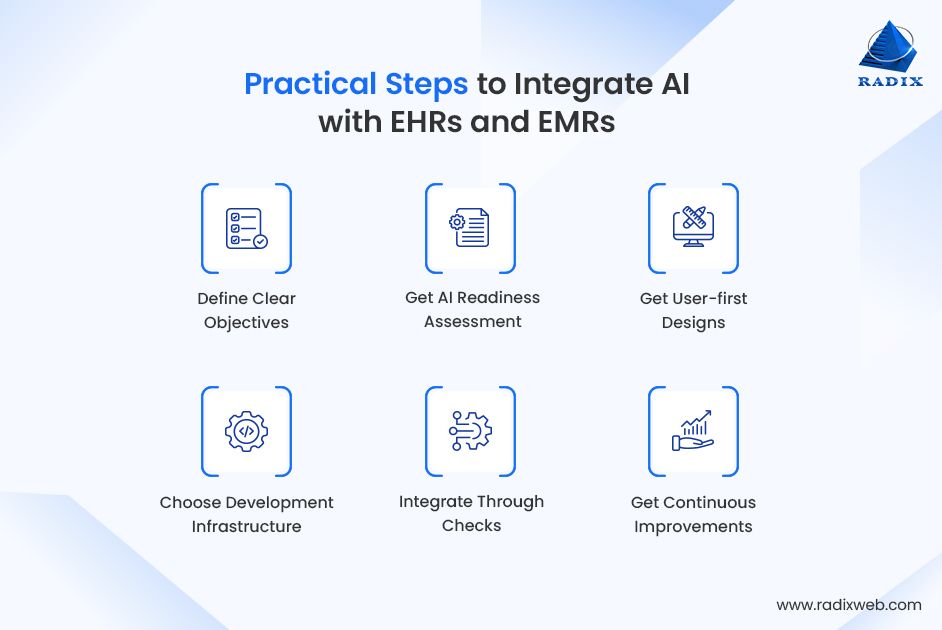
Define Clear Objectives
Pinpoint your desired business objective from the AI-EHR integration. Define clear goals like enhancing diagnostic speed, professional upskilling, increasing patient satisfaction or reducing administrative work. Integrate automation for resource scheduling, and AI to uncover hidden links in data.
Conduct AI Readiness Assessments
Your core integration strategy should stem from AI consultations that helps determine EHR/EMR AI readiness and your business goals. Evaluate your existing EHR workflows against to identify areas where AI can add value. Thoroughly assess the compatibility of AI solutions with external systems; plan global and regional compliance adherences even before designing interfaces.
Build User-first Designs
Building AI capabilities for the healthcare industry should make your human resources’ life easy, not the other way around. Design your interfaces with a native feel and intuitive actions that align with existing EHR workflows, deviations would require time-intensive retraining. Also include solution adaptability across screen sizes, devices etc. and test usability with real users before rollout.
Choose the Best-fit Development Structure
Start with quick-to-launch MVPs that measure usability and gathers feedback from clinicians and admin staff on essential features. Custom prototypes and MVP development helps you gather realistic insights without risking cost and reputation. Next choose the suitable integration approach for your EHR – custom solutions, API-led or AI modules.
Integrate Through Checks
Build safe sandbox environments to test pilot plans before moving to live environments. Constantly check for global and regional compliances (GDPR, HIPAA etc.), maintain strict audit logs, check interoperability with existing EHRs and thoroughly monitor latency logs, data sync accuracy and uptime.
Leave Space for Continuous Improvement
As the markets progress, your AI-led EHRs will fall back in terms of capabilities. You must consider AI integrations as a continuous improvements and not one-time investments. Ensure you help AI-powered capabilities scale across EHR specialities, take a phased rollout approach, deliver role-based training, constantly monitor adoption challenges and expand integrations for future-ready systems.
Navigate Ethical Considerations & Common Challenges in AI-EHR Integrations (and How to Overcome Them)
Having AI-led capabilities in digital records for the healthcare industry is crucial. However, to leverage its realistic benefits, you’ll need to surpass a range of practical ethical considerations and challenges of AI adoption in EHR/EMR software development. Let’s take a quick look at them:
Data Bias: ML algorithms often lead to biased outcomes in predictive models. Ensure your training and historical data is correct, clean and complete. Avoiding data bias helps you maintain fairness in AI-led decisioning.
Reliability: This is also directly linked to training and historical data quality and relevance. Inaccurate or poor-quality data often leads to inaccurate AI outcomes and recommendations.
Responsibility: While there’s a growing trend to attribute every function to AI-led solutions, human intervention often takes a back seat. You must use AI as an enabler and not a decision maker and have human governance at the helm of ethical decisioning in patient care.
Data Security: Data breach incidents do not just cost you your repute, but also bring hefty legal fines. Your healthcare solutions are governed by several regional and global laws; AI should automate EHR compliance on those grounds and trigger alerts in case of discrepancies.
Explainability and Transparency: AI-powered systems must maintain a rigorous log of action for audits. If AI actions for your healthcare solutions aren’t transparent and explanatory, you place your systems in the firing line of AI governance.
Clinical Validation and Evidence-based Practice: Do not integrate AI solutions without validating their capabilities and vulnerabilities. Clinical practice cannot afford missteps, so ensure you test and validate the safety and reliability of AI functions before launching them for actual use.
Human-AI Collaboration: The role of humans in the landscape of AI-powered software solutions has progressed to ethical governance. AI in healthcare regulations should help automate, predict and recommend to complement human professionals. Place human cognition at the helm for ensuring quality care, patient safety and ethical integrities.
Culture of Continuous Training: AI innovations progress at unprecedented speed. Implementing them won’t be enough if your human workforce fails to adapt to changes fast. Address their concerns, relieve mental blocks, encourage them to learn, train and master the workings of AI-led EHRs.
The Future of Healthcare is In Intelligent SolutionsYou could either be one of those businesses who brood over concerns related to AI. Or be one of those forward-thinking ones who realize AI isn’t perfect, but now it’s the right enabler to gain competitive edge. The key here is to know where AI falters, how it blurs ethical lines, the challenges it brings with itself – and then joining hands with seasoned AI experts who’ll help you avoid these pitfalls.At Radixweb, we’ve transitioned multiple healthcare application development projects with diverse AI-powered calibres. Not only can we validate your ideas, but help you implement AI-led solutions in ways that they transform your businesses. Talk to one of our healthtech experts today!
FAQs
How is AI transforming traditional EHR and EMR systems?
What are the main benefits of integrating AI into existing EHR/EMR platforms?
What challenges do healthcare organizations face when integrating AI with EHR/EMR systems?
How can AI integration improve clinical decision support?
Is AI integration with EHR/EMR systems secure and compliant?
How much does it cost to integrate AI into an existing EHR or EMR system?
Which AI technologies are most commonly used in EHR/EMR integration?
How can healthcare providers prepare their EHR/EMR systems for AI adoption?
What’s the future of AI integration in EHR and EMR systems?
Ready to brush up on something new? We've got more to read right this way.